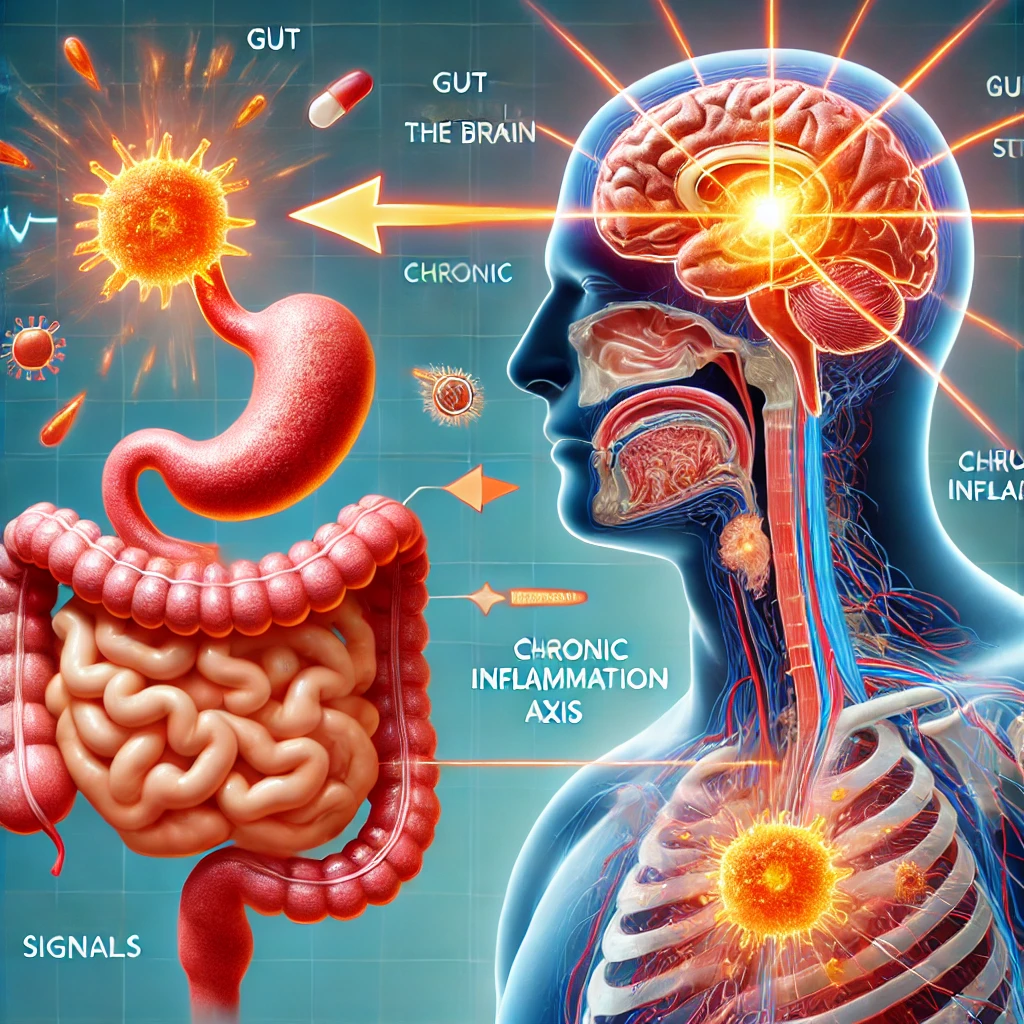
In recent years, the scientific community has increasingly recognized the intricate and influential connection between the gut and mental health. This relationship, often referred to as the “gut-brain axis,” encompasses the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system. The gut-brain axis is a complex, bidirectional communication system that links emotional and cognitive centers of the brain with peripheral intestinal functions. This connection is mediated by multiple systems, including the nervous system, immune system, and endocrine system. Understanding the proven links between gut and mental health is essential for developing new treatments for mental health disorders and improving overall well-being.

The Gut Microbiome: A Brief Overview
At the heart of the gut-brain axis is the gut microbiome, a vast community of trillions of microorganisms residing in the gastrointestinal tract. These microorganisms include bacteria, viruses, fungi, and other microbes that play crucial roles in digestion, metabolism, and immune function. The gut microbiome is highly dynamic and can be influenced by diet, lifestyle, antibiotics, and other environmental factors. Importantly, the composition and diversity of the gut microbiome have been linked to a range of health outcomes, including mental health.
Communication of the Gut-Brain Axis
The Vagus Nerve – the Gut-Brain Axis Super-Highway
The vagus nerve is one of the primary pathways for communication between the gut and the brain. It extends from the brainstem down to the abdomen, innervating various organs along the way. The vagus nerve transmits signals from the gut to the brain, providing information about the state of the gut and influencing brain function. This nerve plays a crucial role in regulating stress responses, mood, and overall mental health.
Neurotransmitters and the Gut
The gut is often referred to as the “second brain” because it produces many of the same neurotransmitters that are found in the brain. For example, serotonin, a neurotransmitter that regulates mood, sleep, and appetite, is predominantly produced in the gut. Approximately 90% of the body’s serotonin is synthesized in the gastrointestinal tract. Other neurotransmitters, such as dopamine and gamma-aminobutyric acid (GABA), are also produced in the gut and play roles in mood regulation and cognitive function.
The Immune System
The gut is a major component of the immune system, with a large proportion of the body’s immune cells residing in the gut-associated lymphoid tissue (GALT). The gut microbiome helps regulate immune function and maintain a balanced immune response. Dysregulation of the immune system and chronic inflammation have been implicated in the development of mental health disorders, such as depression and anxiety.
The Endocrine System
The gut and brain also communicate through the endocrine system, which involves the release of hormones into the bloodstream. The hypothalamic-pituitary-adrenal (HPA) axis is a key part of this system and plays a central role in the body’s response to stress. Dysregulation of the HPA axis has been linked to mental health disorders, and the gut microbiome can influence HPA axis function.
Evidence Linking the Gut-Brain Axis
Depression and Anxiety
Numerous studies have shown a link between gut health and mood disorders such as depression and anxiety. For example, individuals with depression often have altered gut microbiome compositions, characterized by reduced microbial diversity and an imbalance of certain bacterial species. Additionally, studies have demonstrated that manipulating the gut microbiome through diet, probiotics, or fecal microbiota transplantation can influence mood and anxiety levels.
Irritable Bowel Syndrome (IBS) and Mental Health
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. IBS is often comorbid with mental health disorders, such as depression and anxiety. Research has shown that individuals with IBS have distinct gut microbiome profiles compared to healthy individuals. Moreover, treatments targeting the gut microbiome, such as probiotics and dietary interventions, have been shown to improve both gastrointestinal and mental health symptoms in IBS patients.
Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) is a developmental disorder characterized by challenges with social communication, repetitive behaviors, and restricted interests. Gastrointestinal issues are common in individuals with ASD, and research suggests that the gut microbiome may play a role in the disorder. Studies have found differences in the gut microbiome composition of individuals with ASD compared to neurotypical individuals. Additionally, interventions aimed at modifying the gut microbiome, such as probiotics and dietary changes, have shown promise in improving behavioral symptoms in some individuals with ASD.
Schizophrenia
Schizophrenia is a severe mental health disorder characterized by hallucinations, delusions, and cognitive impairments. Emerging research suggests that the gut microbiome may be involved in the pathophysiology of schizophrenia. For example, studies have found differences in the gut microbiome composition of individuals with schizophrenia compared to healthy controls. Additionally, animal studies have shown that manipulating the gut microbiome can influence behaviors and brain function related to schizophrenia.
Mechanisms Underlying the Gut-Brain Axis
Inflammation
Chronic inflammation has been implicated in the development of various mental health disorders. The gut microbiome plays a crucial role in regulating the immune system and maintaining a balanced inflammatory response. Dysbiosis, or an imbalance in the gut microbiome, can lead to increased intestinal permeability (often referred to as “leaky gut”) and systemic inflammation. This inflammation can affect the brain and contribute to the development of mental health disorders.
Metabolites and Neuroactive Compounds
The gut microbiome produces a variety of metabolites and neuroactive compounds that can influence brain function. Short-chain fatty acids (SCFAs), such as acetate, propionate, and butyrate, are produced by the fermentation of dietary fibers by gut bacteria. SCFAs have anti-inflammatory properties and can cross the blood-brain barrier, where they may influence brain function and behavior. Other metabolites, such as tryptophan metabolites, can also affect neurotransmitter production and brain function.
Epigenetic Modifications
The gut microbiome can influence gene expression through epigenetic modifications. Epigenetics refers to changes in gene expression that do not involve changes to the underlying DNA sequence. These changes can be influenced by environmental factors, including the gut microbiome. For example, gut bacteria can produce metabolites that modify histones (proteins around which DNA is wrapped), influencing gene expression in the brain and affecting mental health.
Therapeutic Implications of the Gut-Brain Axis
Probiotics and Prebiotics
Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. Prebiotics are dietary fibers that promote the growth of beneficial gut bacteria. Both probiotics and prebiotics have been studied for their potential to improve mental health. For example, specific probiotic strains have been shown to reduce symptoms of depression and anxiety in clinical trials. Prebiotics, such as fructooligosaccharides (FOS) and galactooligosaccharides (GOS), have also been found to have positive effects on mood and cognitive function.
Diet and Nutrition
Diet plays a crucial role in shaping the gut microbiome and influencing mental health. Diets rich in fruits, vegetables, whole grains, and fermented foods have been associated with a more diverse and balanced gut microbiome. Conversely, diets high in processed foods, sugars, and unhealthy fats can negatively impact gut health and contribute to mental health disorders. Nutritional interventions aimed at improving gut health, such as the Mediterranean diet, have shown promise in improving mood and cognitive function.
Fecal Microbiota Transplantation (FMT)
Sure, this sounds gross. But think of the benefits. Fecal Microbiota Transplantation (FMT) involves the transfer of fecal material from a healthy donor to the gastrointestinal tract of a recipient. FMT has been primarily used to treat Clostridioides difficile infections, but it is also being explored as a treatment for other conditions, including mental health disorders. Preliminary research suggests that FMT can modify the gut microbiome and improve symptoms of depression and anxiety.
Psychobiotics
Psychobiotics are a class of probiotics and prebiotics that specifically target the gut-brain axis and have the potential to improve mental health. The concept of psychobiotics is still relatively new, but early research has shown promising results. For example, certain strains of Lactobacillus and Bifidobacterium have been found to reduce symptoms of depression and anxiety in both animal models and human studies.
Challenges and Future Directions of the Gut-Brain Axis
While the connection between gut and mental health is well-established, there are still many challenges and unanswered questions in this field. One challenge is the complexity and individuality of the gut microbiome. Each person’s gut microbiome is unique, and factors such as genetics, diet, and environment can influence its composition and function. This variability makes it challenging to develop universal treatments targeting the gut-brain axis.
Another challenge is understanding the precise mechanisms underlying the gut-brain connection. While significant progress has been made, more research is needed to fully elucidate how the gut microbiome influences brain function and behavior. Additionally, most studies to date have been correlational, and more experimental and longitudinal studies are needed to establish causality.
Future research should also focus on identifying specific microbial strains and metabolites that are most beneficial for mental health. This knowledge could lead to the development of targeted probiotic and prebiotic therapies. Furthermore, personalized approaches to gut health, taking into account an individual’s unique microbiome, genetic background, and lifestyle, may be more effective in improving mental health outcomes.
Summing up the Gut-Brain Axis
The gut-brain axis represents a fascinating and complex system of communication between the gastrointestinal tract and the central nervous system. The gut microbiome, through its influence on the nervous, immune, and endocrine systems, plays a crucial role in mental health. Understanding the proven links between gut and mental health has significant implications for developing new treatments for mental health disorders and improving overall well-being. As research in this field continues to advance, it holds the promise of unlocking new therapeutic strategies that harness the power of the gut microbiome to support mental health and well-being.
